Acute Painless Vision Loss: The Diseases
Be sure to review normal retina anatomy in the “Anatomy” section of this site in order to better appreciate what is pathologic over here
Retinal Detachment (RD)
Essentially a retina that has been ripped off its base
Pathognomonic words/descriptors:
”Curtain fell over my vision”
“Flashes of light”
“Acutely seeing many new floaters”
•Epidemiology: Pt’s w/ diabetic retinopathy, trauma, myopia
•Signs: Floaters, flashes of light, visual field defects (“curtain falling down over vision”)
•What to do: Refer emergently to ophtho for laser/surgery treatment. If the detachment includes a detached macula, then it requires intervention within a few days. However if the macula is not yet detached, intervention is indicated within hours to prevent the macula from detaching
•Complications: Permanent vision loss if untreated
Retinal Artery Occlusion (RAO)
Essentially a Stroke of the Eye
Pathognomonic words/descriptors:
“Cherry red macula” (Also seen in Niemann Pick and Tay Sachs disease, but not acutely)
“Sudden monocular painless vision loss + carotid bruit”
“Sudden monocular painless vision loss + Afib”
“Hollenhorst plaque” - intra arterial plaque (picture here)
•Epidemiology: Pt’s w/ carotid disease or embolic risk factors
•Signs: Afferent pupillary defect + sudden loss of vision
Central Retinal Artery Occlusion (CRAO): Complete loss of vision
Branch Retinal Artery Occlusion (BRAO): Acute visual field defect
•What to do: This is considered a stroke. Refer to ER emergently for stroke workup. Can perform ocular massage to try to dislodge the plaque but this does not have any evidence of efficacy
•Complications: Vision loss usually permanent. Clot-busting agents (tPA) usually not recommended due to high risk of intracranial bleeding.
Retinal Vein Occlusion (RVO)
Essentially a DVT (deep vein thrombosis) of the Eye
Pathognomonic words/descriptors (commonly seen in ‘Central’ RVO):
“Blood and Thunder retina” aka. Multiple acute flame shaped hemorrhages (as seen in picture here)
“Acute massive papilledema”
•Epidemiology: Older patients with thrombotic risk factors. (diabetes, cardiovascular disease, hypertension, obesity)
•Signs:
Central Retinal Vein Occlusion (CRVO): Sudden blurry distorted vision. Possible Afferent pupillary defect. Blood and Thunder Retina. Papilledema
Branch Retinal Vein Occlusion (BRVO): More subtle. Possible visual field defects, usually no blood and thunder retina or papilledema
•What to do: Urgent referral to retina specialist + systemic workup for cardiovascular risk factors
•Complications: Permanent vision loss variable, commonly occurs due to “neovascularization” of the retina due to ischemia
Amaurosis Fugax
Essentially a TIA (transient ischemic attack) of the eye
Pathognomonic words/descriptors:
Sx of CRAO/BRAO that self-resolve in minutes
May see hollenhorst plaque on fundus exam (as seen in image on right)
•Epidemiology: Older patients with thromboembolic risk factors. Condition can be caused by hypotension, thrombus, embolus, arteritis, or vasospasm
•Signs: Sudden loss of vision that comes back after a few minutes
•What to do: Urgent neuro-vascular and systemic workup for stroke risk factors as well as other etiologies
•Complications: Vision loss transient, but this condition portends an impending stroke or other systemic condition (inflammation, arteritis, etc.)
Retinal Hemorrhage
Bleeding in the retina caused by many etiologies that deserves a careful workup
•Epidemiology: Trauma, sepsis, coagulopathy, hypertension, intoxication, infections, diabetes, artery aneurysm rupture
•Signs: Floaters, vision distortion
•What to do: Urgent referral to retina specialist for medical or surgical management.
A retinal hemorrhage could be the only sign of abusive head trauma, blood dyscrasia, diabetes, hypertension, sickle cell disease, lupus erythematosus, cancer, endocarditis (Roth Spots), and other systemic diseases, thus needs to be worked up
Given the diversity of etiologies, management varies highly by cause
•Complications: Varies by underlying condition
Giant Cell Arteritis (GCA)
Essentially systemic blood vessel inflammation causing rapid ischemia of the optic nerve
Pathognomonic words/descriptors:
“Temporal headache + painless vision loss”
“Polymyalgia rheumatica + vision loss”
“Jaw claudication + vision loss”
“Fever, weight loss, night sweats + vision loss”
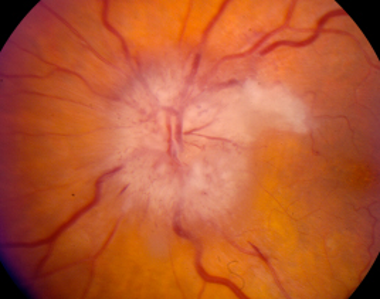
“Chalk white optic disc edema + hemorrhage” (as seen here in picture on right)
•Epidemiology: Female > Male, age 50+, associated with polymyalgia rheumatica
•Signs: Fever, weight loss, night sweats, fatigue, unilateral temporal headache and jaw claudication, hard and tender temporal artery, painless vision loss
•What to do: Emergent high dose corticosteroid administration if suspected and ER referral for diagnosis (elevated ESR + Temporal artery biopsy) and management
•Complications: If untreated – permanent vision loss, cerebral ischemia, aortic aneurysm
Optic Nerve Compression/Neuropathy/Neuritis
Essentially an ominous finding associated with dangerous diseases
Pathognomonic words/descriptors:
Papilledema
Acute Color vision changes
Optic nerve pallor
Afferent Pupillary Defect
•Causes:
Ischemic:
Arteritic (inflammation): Giant cell arteritis, other vasculitis
Non arteritic (impaired circulation): Htn, DM
Infectious: Neurosyphilis
Optic Neuritis: Nerve inflammation. Lead point for multiple sclerosis
Compressive: Tumors, infections, thyroid eye disease. Pseudotumor Cerebri (aka Idiopathic Intracranial Hypertension)
Infiltrative: Sarcoidosis
Traumatic: Physical injury (e.g. bullet) or surgical complication
Nutritional/Toxic: B12 deficiency/pernicious anemia, Methanol
Hereditary/Genetic/Mitochondrial: Leber’s Hereditary Optic Neuropathy
•Signs: Afferent pupillary defect. Loss of color vision, visual field defects, pain, characteristic optic nerve findings
•What to do: Urgent workup by ophthalmology and possible multidisciplinary care team
•Complications: If untreated – permanent vision loss and systemic effects depending on underlying disease