Eye Anatomy
Key Structures and Pathologically Relevant Principles
Basic Eye Anatomy
A review of basic eye structures, with focus on physiologic and pathologic correlates.
The Retina
A review of the retinal layers, vessels, optic nerve and basic optical coherence tomography
Gonioscopic Anatomy
For advanced students. Review of gonioscopy and the various grading systems used to describe the angle
Basic Eye Anatomy
Click above to see a video that uses diagrams and a cadaveric dissection of the eye to explore basic eye anatomy
Structures of the Eye
The eye consists of the following structures, as detailed in the video:
External eye and adnexa
Eyelids and lashes
Lacrimal (tear) apparatus
Conjunctiva
Sclera
Cornea
Anterior chamber
Ciliary body and aqueous drainage system
Iris
Lens
Vitreous
Retina and Optic Nerve
Below, find an explanation of each anatomical part from the above video with physiologic and pathologic correlates. Only the most important anatomical details are listed, alongside web links to videos and diagrams (each underlined text is a link)
External eye and adnexa
The eye is attached to six muscles that provide movement
The eyelid is opened by Superior Tarsal (Muller’s) muscle and the levator palpebrae. It is closed by the orbicularis oculi muscle
The tarsal plate is a fibrous layer in the eyelid that provides lid support. They contain Meibomian glands that provide oily secretions for tear film
Resources:
Review external landmarks and eye muscles through this diagram quiz
Explore the cross section and external diagram of an eyelid
Learn about tear production and the lacrimal apparatus here
Sclera
Dense fibrous, collagenous structure which gives rigidity to the eye
Its outermost layer is called episclera, which is a vascularized connective tissue
Anterior Chamber
Empty space between cornea and iris filled with aqueous humor
Decreased deepness of the anterior chamber increases a patient’s risk of angle closure glaucoma
Can be examined in detail through gonioscopy (see below)
Iris, Ciliary Body and Choroid (Collectively Known as Uvea)
The uvea is a pigmented and highly vascular layer that can become inflammed (uveitis)
The choroid supplies nutrition to the outer layers of the retina (up to the outer plexiform layer - see retina anatomy)
The ciliary body is the anterior continuation of the choroid. It produces aqueous humor and helps with accommodating the lens via the ciliary muscle
The iris a circular diaphragm that constricts (parasympathetic) and dilates (sympathetic) to control the amount of light through the pupil
The iris can bow forward, causing angle closure glaucoma or press against the lens, causing pupillary block glaucoma
Conjunctiva
A thin translucent mucous membrane that consists of two parts:
Palpebral (on the eyelid)
Bulbar (covering the eyeball)
Cornea
Is the most densely innervated tissue in the body (hence injury is extremely painful)
Helps in refracting light
Consists of 5 layers, which can be visualized in a slit lamp exam, from outermost to innermost:
Epithelium: contains stem cells at the limbus and can regenerate
Bowman’s membrane: acellular layer that cannot regenerate following trauma
Stroma: Comprises 90% of corneal thickness
Descemet’s Membrane: Is the basement membrane of the endothelium
Endothelium: Single hexagonal layer of cells (density: 5000 cells/sq mm at birth; declines with age) that dehydrate the cornea. This layer cannot regenerate and damage causes corneal edema once cell counts are below 500 cells/sq mm
Lens
Is a transparent biconvex structure that refracts light onto the retina. It consists of three parts:
Capsule: is an envelope that holds the lens cortex and nucleus in place, like a plastic bag. It is attached to zonules of the ciliary body to allow for lens contraction and relaxation
Cortex: is the outer portion of the lens. It becomes opacified in spoke fashion in cortical cataracts
Nucleus: the central portion of a lens. In a nuclear cataract, the lens becomes hazy and opaque centrally
Vitreous
Inert, transparent, jelly like structure that fills the eyeball behind the lens
Supplies nutrients to the lens and retina
Liquefies with age, causing floaters
Retina Anatomy and Images
Histological cross section of the retina
Layers of the Retina: An Overview from Inner to Outer Retina (Anterior to Posterior):
Inner limiting membrane: Is the structural interface between the vitreous and retina
Retinal Nerve Fiber Layer: Consists of axons of the optic nerve as they course across the retina
Ganglion Cell Layer: Contain cells that integrate information from intermediate cells in the retina that receive information from the photoreceptors and create action potentials to be propagated along the nerve fiber axons
Inner Plexiform Layer: Layer consisting of the dendrites of retinal ganglion cells and cells of the inner nuclear layer
Inner Nuclear Layer: Contains 3 types of cells (bipolar, amacrine, horizonal cells) that compute and integrate signals from photoreceptors
Outer Plexiform Layer: Consists of dendrites connecting photoreceptors and inner nuclear layer cells
Outer Nuclear Layer: Contain portions of the photoreceptors
External Limiting Membrane: Landmark separating the photoreceptor nucleus from the metabolic (inner) segment and light sensing (outer) segment of the cell (see here for diagram)
Photoreceptor layer: Contains the inner and outer segments of the photoreceptor
Retinal Pigment Epithelium: Layer responsible for nourishing the retina, prevent reflection on the retina, and acts as a blood-eye barrier
See this excellent video if further interested in the electrical circuitry of retinal signal processing
Optical Coherence Tomography Imaging of the Retina (for advanced students)
Optical Coherence Tomography (OCT) is an imaging test that ophthalmologists use in clinic to visualize the histology of the retinal cell layers discussed above. It can be used to detect:
Thinning of certain retinal layers
Fluid/bleeding in various regions of the retina
Accumulation of drusen in the retina (see section on age related macular degeneration)
Extra membranes forming on the retina
Retinal vasculature (in the form of performing non invasive angiography of retinal vessels, known as OCT angiography)
On an OCT scan of the retina, the histologic layers are clearly delineated, as seen in this scan of the central retina, known as the macula:
Interpreting OCT scans is an integral part of ophthalmology. If interested in exploring the basics of OCT scans further, see the following resources:
EyeGuru’s quiz modules on basic OCT pathologies (especially good for learning basic retinal diseases, requires free registration)
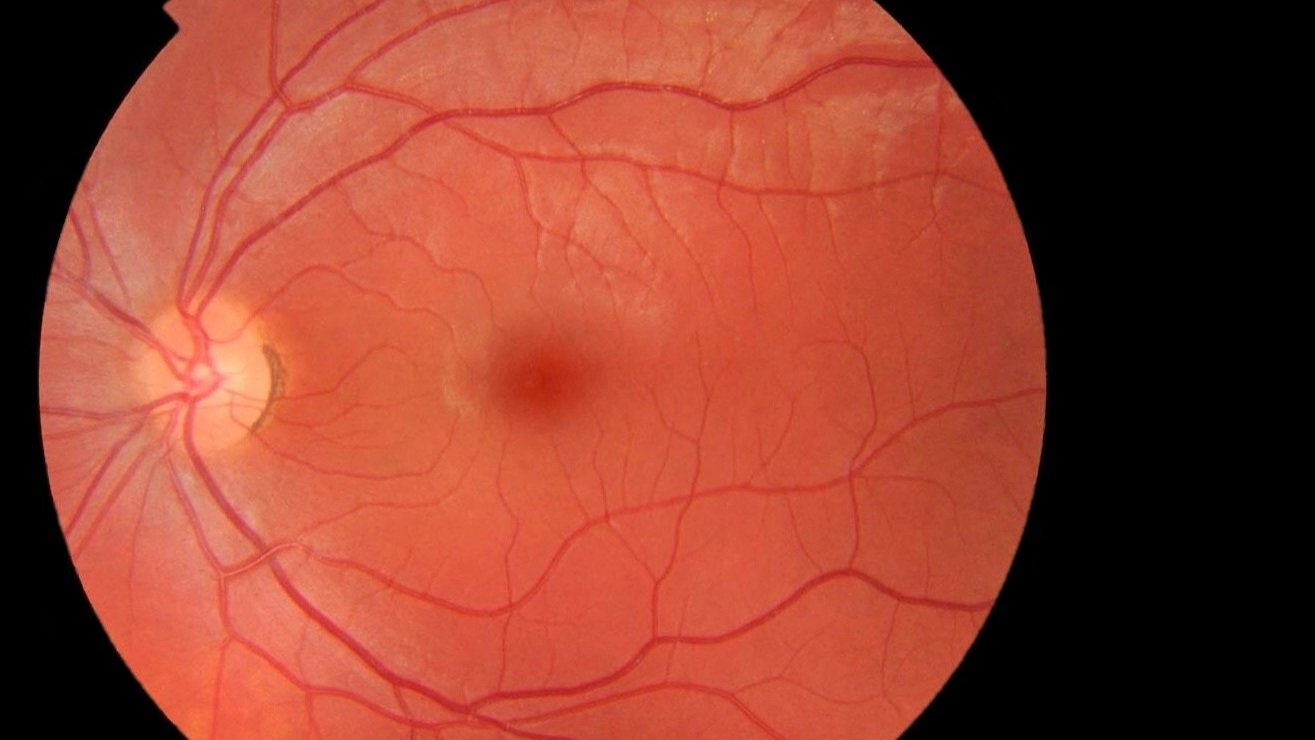
Retinal Photography
Understanding how the healthy retina looks on direct visualization is crucial to both the ophthalmologist or the non-ophthalmologist using direct ophthalmoscopy.
Color fundus photo of the right eye centered on the macula. The vessels are flat and normal sized without evidence of AV nicking or micro-aneurysms. The periphery is normal, without exudate or pigmentary changes. The macula is flat. The optic disk is sharp, normally colored and has a cup:disc ratio of 0.3
Descriptive characteristics of the healthy retina:
Type of image:
Color fundus photo shows the eye with its normal color. It can be contrasted by other studies such as fundus autofluorescence or fluorescein fundus angiography.
Laterality of the eye is determined by looking at the optic nerve, which is always nasal. As a quick rule of thumb, the position of the nerve in the picture (left or right) corresponds to the eye being observed.
Centering of the image is also important. Some images can be focused on the optic disc or be wide-field images
Optic Nerve
Color: A healthy nerve should be pink. Disc pallor could be a sign of atrophy
Sharpness/Border: A sharp border of the disc is normal. Blurred discs (papilledema) could be caused by inflammation or increased intracranial pressure
Cup-to-disc ratio: a ratio of above 0.7 or a difference >0.2 between eyes is considered pathologic, usually indicative of glaucoma. See discs with various C/D ratios here
Hemorrhage: Bleeding on the disc can also be an indicator of glaucoma
Retinal Vessels:
In a healthy eye, the caliber of retinal veins to arteries is 3:2
Retinal neovascularization (on the optic disc, elsewhere) can be a sign of various diseases
Various features of the vessels, such as aneurysms, AV-nicking, and arteriolar narrowing can be suggestive of systemic disease such as hypertension
Retinal Hemorrhage:
Can be found in three locations:
Preretinal (between vitreous and retina). Is classically boat shaped (additional image)
Intraretinal (can be flame shaped if superficial and at the level of the nerve fiber layer or dot-blot which is in the deeper retina)
Subretinal (behind the neurosensory retina - note the retinal vessels are intact looking)
See this resource from UMichigan for more examples and details on retinal hemorrhages
Other Common “Yellow-white appearing“ Findings:
Cotton wool spots: Soft yellow spots corresponding to various diseases such as diabetes
Hard Exudates: More defined patches of lipoprotein filled macrophages that have extravasated. Also associated with diabetes
Drusen: Yellow flecks representing dead retinal pigment epithelial cells
Gonioscopy
Coming soon








